My friend ST told me that on hot days like today, she always wants to wear a sleeveless top. But after a nasty eczema flare-up, she has brown patches and scratch lines on her arms and shoulders, making her think twice.
She also worries that the eczema scars are now permanent. Did she do irreversible damage by scratching so much?
Well, she’s not alone. If your first reaction is worry or embarrassment, then I have good news. Most of what we call “eczema scars” are not true scars. They’re post‑inflammatory changes. And with the right approach, they will usually fade.
What You’re Seeing: The Types of “Eczema Scars”
There are actually different types of scars. Understanding what’s actually on your skin makes it easier to treat, and also less scary. Below are the common post‑eczema marks you’ll see, what causes them, how long they usually last, and what helps them fade.
Brown/dark patches: Post‑Inflammatory Hyperpigmentation (PIH)

PIH looks like tan, brown or grey patches and is especially common in medium to deeper skin tones. It happens when inflammation from an eczema flare-up tells your body to make more pigment cells to produce extra melanin, which then deposits in the skin.
Good news: PIH is not a true scar. It’s a colour change that usually fades as the skin remodels. Expect gradual improvement over months; many people see noticeable fading in roughly 3–24 months depending on depth and skin tone.
You can speed this up and reduce darkening by using daily broad‑spectrum SPF sunscreen, avoiding heat and further irritation, and introducing gentle brighteners (niacinamide, azelaic acid or vitamin C derivatives) once the skin is calm.

Pink/red patches: Post‑Inflammatory Erythema (PIE)
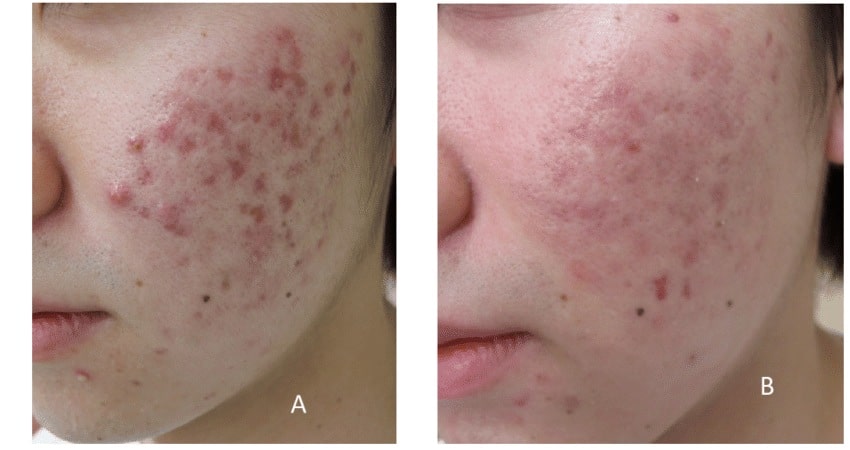
PIE shows as pink or red patches and is caused by dilated or persistent superficial blood vessels after inflammation. It’s more visible on lighter skin tones, but anyone can have it after a bad flare.
PIE often settles within a few months (commonly 3–12 months) as vascular reactivity reduces. Persistent redness can respond well to vascular‑targeting treatments such as pulsed dye laser (PDL) or other vascular lasers if you see a dermatologist, but start with gentle anti‑inflammatory care, strict sun protection and barrier repair first.
Scratch lines and thickened skin: Excoriation & Lichenification

These are the marks you get from repeated rubbing and scratching. Excoriations look like straight lines of scratch tracks, scabs or darker lines. Lichenification is the leathery, thickened skin that comes from chronic rubbing.
The texture and lines usually improve once the itch–scratch cycle is controlled and the barrier is rebuilt. That means itch management (topical treatments, emollients, gloves/sleeves at night), moisturising generously, and protecting the area from further trauma. Remember to be patient as it may take weeks to months as inflammation calms and the skin regenerates.
True Scars (Less Common): Atrophic, hypertrophic, keloid
True scarring is less common after eczema but can happen with deep injury, infections, or prolonged untreated damage. Types include:
- Atrophic scars: shallow dents or pits where tissue was lost.
- Hypertrophic/keloid scars: raised, firm, sometimes itchy or painful lumps.
These are more likely after deep wounds or infections and commonly appear on the chest, shoulders and areas prone to tension. True scars often need targeted therapies such as injections for hypertrophic/keloid scars, or microneedling/lasers for atrophic ones.
If you’re unsure which type of mark you have, a simple rule of thumb helps: colour changes (brown/pink) are usually reversible with time and gentle care; texture changes (thickening, pits, raised lumps) may need more targeted treatment. Whatever you’re seeing, the first step is the same: calm the inflammation, protect skin from further damage, then rebuild the barrier so your skin has the best chance to heal.
Why These Marks Happen: The Itch–Scratch–Inflammation Loop
The Itch–Scratch–Inflammation Loop
Eczema marks are usually the visible result of a cycle that keeps repeating until it’s broken. It starts with skin barrier breakdown → inflammation → itch → scratch → more damage.
Here’s how each step creates the marks you see:
When the skin barrier is damaged (loss of lipids, moisture and protection), irritants and microbes get through more easily. The immune system responds with inflammation, releasing chemical signals that both dilate tiny surface blood vessels (which shows as redness or PIE) and stimulate pigment cells to produce extra melanin (which becomes PIH). In short: inflammation changes colour and tone.
Scratching makes things worse. Every scratch creates tiny micro‑tears and mechanical trauma that boost inflammation locally. That extra inflammation encourages more pigment production and can thicken the skin over time. This is how excoriation lines and lichenification form. Repeated rubbing also reinforces the habit loop: itch → scratch → temporary relief → more itch.
Infection is the wildcard that deepens the problem. Bacteria (Staph is common in eczema) or other infections delay normal healing, crank up inflammation and raise the chance of deeper tissue damage, which increases the risk of true scarring (hypertrophic or atrophic). Signs of infection to watch for are spreading redness, warmth, increasing pain, pus, or fever. If you see these, seek medical advice.
Will They Be Permanent? What to Expect
The short answer: most post‑eczema marks are not permanent. With consistent calming care, strict daily SPF and barrier repair, PIH, PIE and lichenified areas usually improve over time. But true scarring from deep excoriations, untreated infections, or keloid/hypertrophic responses may persist without targeted treatment. So get professional advice if you want to get rid of those.
Use the checklist below as your daily playbook. Start by calming active inflammation, then protect and rebuild the barrier so healing can happen.
Step 1: Settle active eczema first
Start simple. When skin is red, weepy or cracked, avoid anything that can sting or strip.
- Use a gentle, fragrance‑free cleanser (cream or syndet). Pat dry and don’t rub.
- Avoid any physical or chemical exfoliation on active lesions (no scrubs, peels or retinols until fully calm).
- Be liberal with emollients: apply often and in thick layers to damp skin. Pure emu oil is a good option for deep moisture and calming; use it after cleansing while skin is still slightly damp.
- Use prescribed anti‑inflammatories (topical steroids, calcineurin inhibitors or as advised by your doctor) during flares as they reduce inflammation that drives PIH/PIE. Follow your prescriber’s instructions.
Step 2: Block triggers daily
Exposure to sun, heat, sweat, dust mites and other allergen can trigger a new round of flare-up, which causes more pigment changes and slow healing.
- Use a broad‑spectrum mineral (physical) sunscreen SPF 30+ every morning. Apply generously and reapply every 2 hours if you’re sweating or outdoors.
- Wear UPF clothing, wide‑brim hats and seek shade when possible.
- Cool down after exercise or sweating: change out of damp clothes, use cool compresses, and avoid prolonged heat exposure which can trigger flares and deepen PIH.
- Apply shielding lotion like Gloves In a Bottle to add daily protection for your hands.
Step 3: Rebuild the barrier
A healthy barrier is the foundation for fading marks.
- Choose moisturisers that contain ceramides, glycerin, hyaluronic acid, or use pure emu oil as a deeply penetrating emollient. These ingredients restore lipid balance and hold moisture.
- Use the “soak and seal” method: pat skin lightly after showering and apply your emollient within 3 minutes. This traps moisture in while the skin is still damp.
- On very dry patches, add an occlusive (petrolatum, ointment or a thicker balm) on top to lock everything in overnight.
Step 4: Break the scratch cycle, especially at night
Stopping scratching is one of the fastest ways to prevent marks from becoming permanent.
- Keep nails short and smooth to reduce damage from unconscious scratching.
- Wear eczema gloves, sleep sleeves or mittens at night to prevent nocturnal scratching and protect healing skin. These are simple, practical tools that make a big difference.
- Use cool compresses or a cold pack for intense itch instead of scratching.
- For severe itch or persistent sleep‑time scratching, ask your clinician about wet wrap therapy. It’s effective but should be done under guidance.
Step 5: Even out your skin tone gently
Once inflammation is quiet, you can introduce gentle tone‑evening ingredients slowly and one at a time.
- For PIH (brown patches): consider niacinamide, low‑strength azelaic acid, or gentle vitamin C derivatives.
- For PIE (pink/red): keep the focus on anti‑inflammatory care, strict sun protection and barrier repair.
- Never layer multiple strong actives at once and stop any product that causes stinging or new redness.
Step 6: Support healing from the inside
Good nutrition and lifestyle habits speed repair and reduce flare triggers.
- Eat an anti‑inflammatory plate: oily fish or flax for omega‑3s, colourful vegetables and fruits for vitamin C, and zinc‑rich foods (pumpkin seeds, legumes) to support tissue repair.
- Stay hydrated, prioritise quality sleep, and manage stress with simple routines. Stress can provoke flares and delay healing.
- Track personal triggers (heat, sweat, certain fabrics, or food) in a diary so you can reduce repeat flares that lead to new marks.
Frequently-Asked Questions
Eczema Scars Will Go Away
Most post‑eczema marks are not permanent. They’re the skin’s response to inflammation. And with calm, protective care they usually fade.
The simple, practical formula to follow is this:
- Calm inflammation: stop the cycle of flare and scratch.
- Protect from UV and heat: prevent darkening and further irritation.
- Rebuild the barrier: restore moisture and resilience so the skin can heal.
- Be consistent: results take weeks to months, not days.
Stick with that plan and you’ll be giving your skin the best chance to recover.
You deserve to feel confident in your skin again. Start small, stick with the basics, and be patient. Healing is a process!
Gentle products from Skinshare.sg
- 100% Pure Australian Emu Oil: our flagship, single‑ingredient oil for deep hydration and barrier support
- Eczema gloves, arm/leg sleeves and mittens: simple way to stop night time scratching and keep emollients in place overnight. Perfect to pair with emu oil or a heavier barrier cream
- Fragrance‑free cleansers: non‑stripping, gentle cleansers to avoid re‑irritation
- Sunscreen: broad‑spectrum mineral SPF (zinc/titanium) to prevent PIH darkening and protect healing skin
If you’d like us to feature your story or routine on Skinshare.sg, let me know by clicking the “chat” button to start a WhatsApp. Sharing real progress helps our community learn what works!
